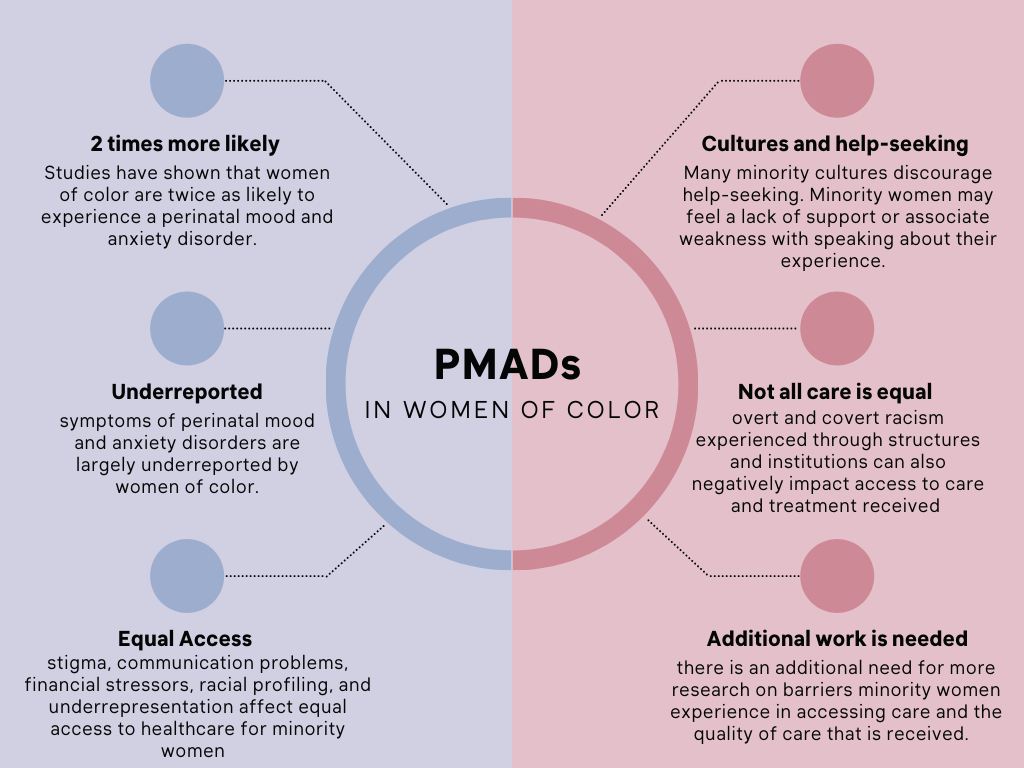
Perinatal mood and anxiety disorders (PMADs) are experienced by women and birthing people of all races and ethnicities, and across all cultures worldwide. Yet in the US, women and parents of color, and parents who identify with sexual and gender minorities experience a significant disparity in the diagnosis and treatment of PMADs.
In one study that examined postpartum mental health care in almost 30,000 women with Medicaid insurance, half as many Black and Latina mothers initiated postpartum mental health treatment as white mothers, and fewer Black and Latina mothers received adequate follow-up treatment or continued mental health care than white women (Kozhimannil et al., 2011). Mothers of color experience postpartum depression at a rate of 38% compared to up to 21% of all new mothers (Gress-Smith et al., 2012; Wisner et al., 2013). Up to one-third of Latina and Black women experience symptoms of anxiety during pregnancy (Ponting et al., 2022).
The increased rates of depression and anxiety can be directly related to discrimination and structural oppression that leads to increased financial, relationship related, and general stress during the perinatal period (Liu et al., 2016; Rosenthal & Lobel, 2011). All women of color and women with low-income are less likely to be screened for postpartum depression than white women and women of higher income brackets (Sidebotton et al., 2020; Declercq et al., 2021). Nearly 60 percent of Black and Latina mothers do not receive any treatment or support services for perinatal mental health (Kozhimannil et al., 2011). In small cities and rural communities, postpartum depression is 40% greater among Latina mothers, and 80% greater among Black mothers than white mothers in similar communities (Ceballos et al., 2017).
The perinatal experiences of birthing people who identify with sexual and gender minorities are under-studied and under-reported. In the UK, birth registrations identify that lesbian couples are one of the fastest growing groups within maternity services, and pregnant trans men are also a growing population within maternity services. Researchers revealed lesbian women in the postpartum period reported a higher prevalence of PMADs and increased rates of attempting/considering suicide (Darwin & Greenfield, 2019). Bisexual women in the postpartum period reported an increased risk of PMADs if currently partnered with a male versus a female (Goldberg et al., 2020). Many birthing people do not report their sexual and and gender orientation to their healthcare providers for fear of discrimination.
Birthing people who identify as BIPoC and/or sexual and gender minorities face many barriers to seeking mental health care treatment, some of which include:
1. High cost of mental health care.
· Birthing people who identify as BIPoC and/or sexual and gender minorities are more likely to have inadequate or no health care insurance.
2. Cultural stigma of mental illness.
· Some cultures and families do not recognize the legitimacy of mental illness and may view individuals who experience mental illness as weak or at fault.
3. Distrust of the medical community.
· Birthing people who identify as BIPoC and/or sexual and gender minorities who have experienced racism or discrimination from previous healthcare encounters may be hesitant to seek subsequent care.
Bringing awareness to the mental health disparities experienced by BIPoC and/or sexual and gender minorities is not enough to create positive and sustained change. Several community-based organizations exist that serve to help birthing people who identify as BIPoC and/or sexual and gender minorities find culturally sensitive mental health care.
· The Perinatal Mental Health Alliance for People of Color is an organization within Postpartum Support International that provides education and support for perinatal mental health care providers of color.
· Queering Parenthood provides mental health information and resources for all families who identify with sexual and gender minorities, as well as education for providers regarding culturally sensitive care.
Birthing people who identify as BIPoC and/or sexual and gender minorities and their families can find culturally sensitive care at Connections Wellness Group with our diverse group of providers.
References
Ceballos, M., Wallace, G., & Goodwin, G. (2017). Postpartum depression among African American and Latina mothers living in small cities, towns, and rural communities. Journal of Racial and Ethnic Health Disparities, 4(5), 916-927. https://doi.org/10.1007/s40615-016-0295-z
Darwin, Z., & Greenfield, M. (2019). Mothers and others: The invisibility of LGBTQ people in reproductive and infant psychology. Journal of Reproductive and Infant Psychology, 37(4), 341-343. https://doi.org/10.1080/02646838.2019.1649919
Declercq, E., Feinberg, E., & Belanoff, C. (2022). Racial inequities in the course of treating perinatal mental health challenges: Results from listening to mothers in California. Birth, 49(1), 132-140. https://doi.org/10.1111/birt.12584
Goldberg, A. E., Smith, J. Z., & Ross, L. E. (2020). 4. Postpartum Depression and Anxiety in Male-Partnered and Female-Partnered Sexual Minority Women. In Marriage and Health (pp. 53-70). Rutgers University Press.
Gress-Smith, J. L., Luecken, L. J., Lemery-Chalfant, K., & Howe, R. (2012). Postpartum depression prevalence and impact on infant health, weight, and sleep in low-income and ethnic minority women and infants. Maternal and Child Health Journal, 16, 887–893. https://doi.org/10.1007/s10995-011-0812-y
Kozhimannil, K. B., Trinacty, C. M., Busch, A. B., Huskamp, H. A., & Adams, A. S. (2011). Racial and ethnic disparities in postpartum depression care among low-income women. Psychiatric Services, 62(6), 619-625. https://doi.org/10.1377/hlthaff.2009.1075
Liu, C. H., Giallo, R., Doan, S. N., Seidman, L. J., & Tronick, E. (2016). Racial and ethnic differences in prenatal life stress and postpartum depression symptoms. Archives of Psychiatric Nursing, 30(1), 7-12. https://doi.org/10.1016/j.apnu.2015.11.002
Rosenthal, L., & Lobel, M. (2011). Explaining racial disparities in adverse birth outcomes: Unique sources of stress for Black American women. Social science & medicine, 72(6), 977-983. https://doi.org/10.1016/j.socscimed.2011.01.013
Wisner, K. L., Sit, D. K., McShea, M. C., Rizzo, D. M., Zoretich, R. A., Hughes, C. L., … & Hanusa, B. H. (2013). Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. JAMA psychiatry, 70(5), 490-498. https://doi.org/10.3410/f.718030385.793480195