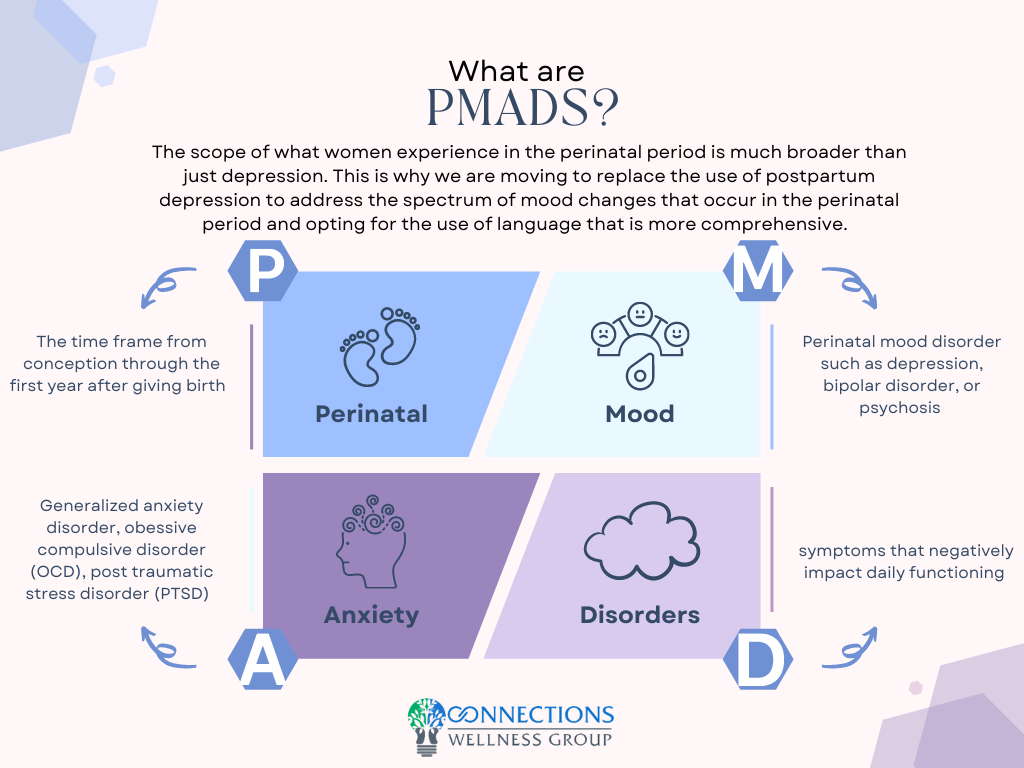
Up to 1 in 5 women experience perinatal mood and anxiety disorders (PMADs) (Weisner et al., 2013). The more familiar term, postpartum depression, is being replaced with PMADs because mood and anxiety disorders can occur at any time in the perinatal period from conception to one-year post-birth. Up to one in ten men experience PMADs.
PMADs are also the number one cause of preventable pregnancy-related deaths (Trost et al., 2021). Untreated and undertreated PMADs represent an annual cost of $14 billion annually, or $32,000 per mother-infant pair.
The United States Preventative Task Force (2019) identified several risk factors for developing PMADs including,
“personal or family history of depression, history of physical or sexual abuse, having an unplanned or unwanted pregnancy, current stressful life events, pregestational or gestational diabetes, and complications during pregnancy (e.g., preterm delivery or pregnancy loss). In addition, social factors such as low socioeconomic status, lack of social or financial support, and adolescent parenthood have also been shown to increase the risk of developing perinatal depression.”
Certain populations are more at risk of developing PMADs including those living in a rural area, women under the age of 19, women with under 12 years of education, unmarried women, Black/African American women, women of American Indian/Alaska Native heritage, birthing people who identify with sexual and gender minorities, women who are immigrants, and immigrant and US-born Latinas/Latinx (USPTF, 2019; Dagher et al., 2021; Lara-Cinisomo et al., 2018; Nidley et al., 2019; Silverman et al., 2018; Xiong & Deng, 2020).
The actual rates of PMADs could be much higher. A systematic review conducted in 2016 (Cox et al.) revealed that up to 50% of women do not receive a correct diagnosis for PMADs. The authors also identified that of women who were diagnosed with a PMAD, only 8.6% of women with depression during pregnancy and 6.3% of women with postpartum depression received adequate treatment.
Untreated or undertreated PMADs have detrimental short and long-term health impacts for both mother and baby with infanticide, homicide, and suicide being the ultimate costs. Up to 17% of maternal suicide occurs during pregnancy through 42 days postpartum, while 83% of maternal suicide occurs between 43 to 356 days postpartum (CA-PMR Report).
Clearly, maternal mental health should be a national health priority. Mental health is essential to the overall health of families. No parent should needlessly suffer from PMADs. Evidence-based treatment and help are available.
References
California Pregnancy-Related Maternal Mortality Review (2019). CA-PMR Report: Pregnancy-Associated Suicide, 2002-2012.
Cox, E. Q., Sowa, N. A., Meltzer-Brody, S. E., & Gaynes, B. N. (2016). The perinatal depression treatment cascade: baby steps toward improving outcomes. The Journal of clinical psychiatry, 77(9), 20901. https://doi.org/10.4088/jcp.15r10174
Dagher, R. K., Bruckheim, H. E., Colpe, L. J., Edwards, E., & White, D. B. (2021). Perinatal depression: challenges and opportunities. Journal of Women’s Health, 30(2), 154-159. https://doi.org/10.1089/jwh.2020.8862
Lara-Cinisomo, S., Clark, C. T., & Wood, J. (2018). Increasing diagnosis and treatment of perinatal depression in Latinas and African American women: addressing stigma is not enough. Women’s Health Issues, 28(3), 201-204. https://doi.org/10.1016/j.whi.2018.01.003
Nidey, N., Tabb, K. M., Carter, K. D., Bao, W., Strathearn, L., Rohlman, D. S., … & Ryckman, K. (2020). Rurality and risk of perinatal depression among women in the United States. The Journal of Rural Health, 36(1), 9-16. https://doi.org/10.1111/jrh.12401
Silverman, M. E., Reichenberg, A., Savitz, D. A., Cnattingius, S., Lichtenstein, P., Hultman, C. M., … & Sandin, S. (2017). The risk factors for postpartum depression: A population‐based study. Depression and anxiety, 34(2), 178-187. https://doi.org/10.1002/da.22597
Trost, S. L., Beauregard, J. L., Smoots, A. N., Ko, J. Y., Haight, S. C., Moore Simas, T. A., … & Goodman, D. (2021). Preventing Pregnancy-Related Mental Health Deaths: Insights From 14 US Maternal Mortality Review Committees, 2008–17: Study examines maternal mortality and mental health. Health Affairs, 40(10), 1551-1559. https://doi.org/10.1377/hlthaff.2021.00615
Wisner, K. L., Sit, D. K., McShea, M. C., Rizzo, D. M., Zoretich, R. A., Hughes, C. L., … & Hanusa, B. H. (2013). Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. JAMA psychiatry, 70(5), 490-498. https://doi.org/10.3410/f.718030385.793480195
Xiong, R., & Deng, A. (2020). Prevalence and associated factors of postpartum depression among immigrant women in Guangzhou, China. BMC Pregnancy and Childbirth, 20(1), 1-7. https://doi.org/10.1186/s12884-020-02946-4